Table of Contents
ToggleAt 10:00 a.m., Penelope entered the world without a cry.
There was no rush of pink skin. No strong wail announcing her arrival. No immediate relief. Instead, there was silence. Stillness. And a shade of blue no parent ever forgets.
Her mother, Verity, knew in that instant something was wrong.
What followed over the next hours would become a fight for survival — one defined not only by medical urgency, but by a mother’s refusal to be dismissed.
A Pregnancy That Seemed Perfect — On Paper
Penelope’s story didn’t begin in chaos. In fact, it began in reassurance.
Verity’s pregnancy was closely monitored due to gestational diabetes. From 16 weeks onward, she underwent repeated ultrasounds — more than six in total. Each appointment showed the same comforting image: a flickering heartbeat, a growing baby, professionals nodding with quiet confidence.
Everything looked normal.
But beneath the routine scans and clinical smiles was a mother carrying invisible scars. Verity had suffered two devastating pregnancy losses before Penelope. Those losses had reshaped her understanding of hope. Every scan brought relief — but never certainty.
At the 20-week anatomy scan, she held her breath until the sonographer smiled.
“The heart looks strong.”
For the first time in months, she allowed herself to believe this pregnancy might end differently.
She was wrong — but not in the way anyone expected.
The Moment Everything Changed
Penelope was delivered via cesarean section. The medical team worked efficiently. Calmly.
But there was no cry.
She was small. Limp. And unmistakably blue.
Before any explanation was offered, Verity felt it — a deep, visceral instinct that cut through exhaustion and anesthesia alike. Something was very wrong.
Doctors reassured her quickly. Fluid in the lungs, they said. A common adjustment issue after a C-section. Oxygen would help. There was no need to panic.
But Verity wasn’t a first-time mother. She had held newborns before. She knew the difference between transitional distress and something more dangerous.
And this wasn’t normal.
Within minutes, Penelope was taken to neonatal care. One moment she was in her mother’s arms. The next, she was gone behind swinging doors.
Left in recovery, surrounded by mothers cradling pink, crying babies, Verity felt something close to dread settle in her chest.
Time stretched painfully.
Then her phone buzzed.
The Photo That Confirmed Her Fear
A nurse had sent a photo of Penelope.
The image stole her breath. The color was unmistakable. Blue — not the fleeting bluish tint of a cold newborn, but a deep, worrying shade that no lighting or camera angle could explain away.
Her hands trembling, she called her husband, Mark.
“Show the consultant this photo,” she insisted. “Tell them something is wrong.”
The response came back dismissive. A strange angle. Flash reflection. Nothing concerning.
But Verity’s instinct refused to quiet.
Weak from surgery, still in her hospital gown, she wheeled herself down to neonatal care and demanded someone listen.
That decision may have saved her daughter’s life.
A Diagnosis That Changed Everything
By chance, a pediatric consultant with cardiac expertise was on duty that day. He agreed to examine Penelope more closely.
An echocardiogram was performed.
Within minutes, the atmosphere shifted.
The consultant reached for his phone.
“I will blue-light her now.”
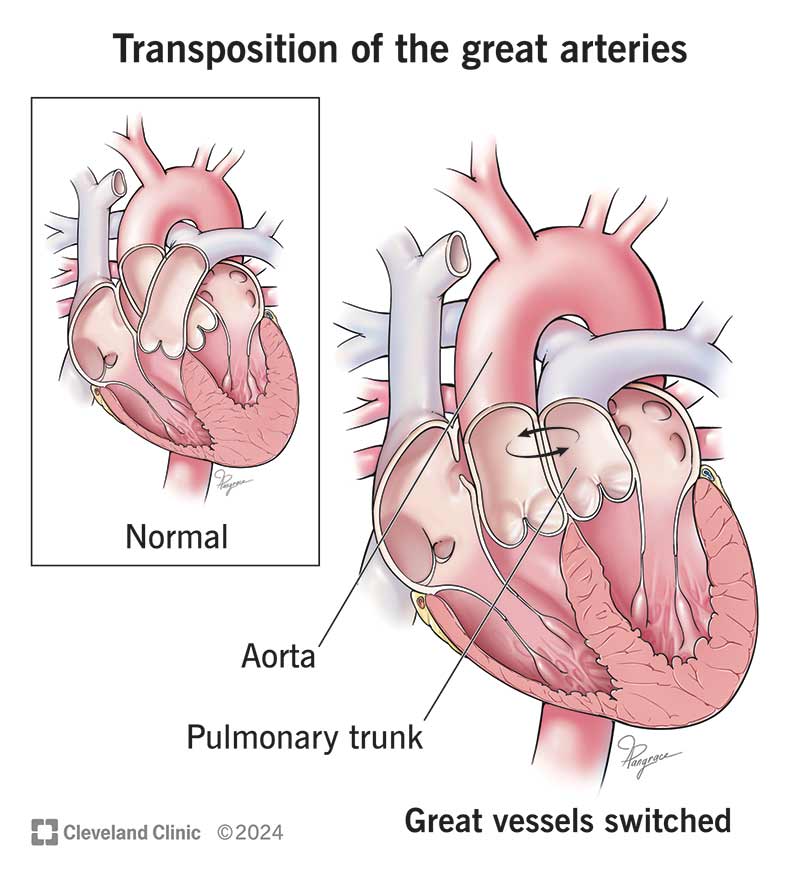
Penelope had Transposition of the Great Arteries (TGA) — a rare and life-threatening congenital heart defect where the two main arteries leaving the heart are reversed. Oxygen-rich blood and oxygen-poor blood circulate incorrectly. Without urgent intervention, survival is impossible.


The consultant chose honesty over comfort.
“Don’t Google it,” he told Verity gently.
He didn’t need to explain further. The urgency in his voice said enough.
Penelope was born at 10 a.m. By 5 p.m., she was in an ambulance racing toward specialist cardiac care in Southampton.
In just seven hours, her parents’ world had shattered and reassembled into something unrecognizable — one ruled by monitors, ventilators, and the terrifying language of survival percentages.
Ten Days Old — Facing Open-Heart Surgery
As further tests were conducted, doctors discovered Penelope’s condition was even more complex than first believed. Multiple abnormalities. Severe instability. A heart already edging toward failure.
She was dangerously small.
At just ten days old, she was scheduled for open-heart surgery.
The surgeon spoke plainly:
Her size made the procedure riskier.
Her heart’s anatomy made it delicate.
Survival could not be guaranteed.
Verity and Mark waited for ten agonizing hours while their newborn lay on an operating table.
Every passing footstep down the corridor made their hearts jump. Every minute felt suspended between hope and devastation.
When the surgery ended, relief came — but it was fragile.
She had survived the operation.
But the fight wasn’t over.
Complications No Parent Is Prepared For
The months that followed tested every ounce of strength they had.
Sepsis.
Blood clots.
Chylothorax.
Strokes.
Multiple additional procedures.
Each new complication reopened the same fear: Is this the moment we lose her?
Days blurred into nights. Machines beeped constantly. Medical terminology became part of daily vocabulary. Hope became measured in oxygen levels and stable readings.
And through it all, Penelope fought.
Tiny. Scarred. Fragile.
But fiercely alive.
After four and a half months in the hospital, she finally came home.
Not healed. Not free from risk.
But alive.
The Questions That Still Linger
Alongside gratitude lived another truth — one far more difficult to process.
Penelope’s heart defect should have been detected during pregnancy.
With more advanced imaging equipment, improved screening standards, or specialized cardiac training, her condition might have been identified in utero. Her delivery could have been planned at a cardiac center. Her first hours could have been controlled, prepared, safer.
Instead, those hours were chaotic and critical.
Verity still carries those unanswered questions. What might have been prevented. What suffering could have been avoided.
There are no clear answers.
But there is purpose.
Today, advocacy has become part of her motherhood. She speaks out about prenatal screening. She urges better training. She encourages parents to trust their instincts — even when professionals offer reassurance.
Because sometimes, instinct sees what machines miss.
Thriving, Laughing — Living
Today, Penelope is thriving.
She laughs. She explores. She grows with a curiosity untouched by the trauma of her earliest days.
The scar across her chest is not hidden.



It is worn proudly — a quiet symbol of survival.
Every milestone feels monumental. Every smile feels earned. Every birthday feels extraordinary.
She is not defined by what she endured.
But she is undeniably shaped by it.
A Story Bigger Than Medicine
Penelope’s survival rests on many things:
Medical skill.
Advanced cardiac surgery.
Resilient anatomy.
Modern neonatal care.
But above all else, it rests on something deeply human.
A mother who refused to be dismissed.
If Verity had accepted reassurance.
If she had doubted herself.
If she had stayed in recovery instead of demanding to be heard —
Penelope might not be here.
Her story is not just about congenital heart disease. It is about listening. About advocacy. About instinct. About the courage to question when something feels wrong.
Because sometimes the difference between tragedy and survival is a single voice refusing to go quiet.
Penelope was born blue and silent.
But today, she laughs loudly.
She is a fighter.
She is a miracle.
She is Penelope.
